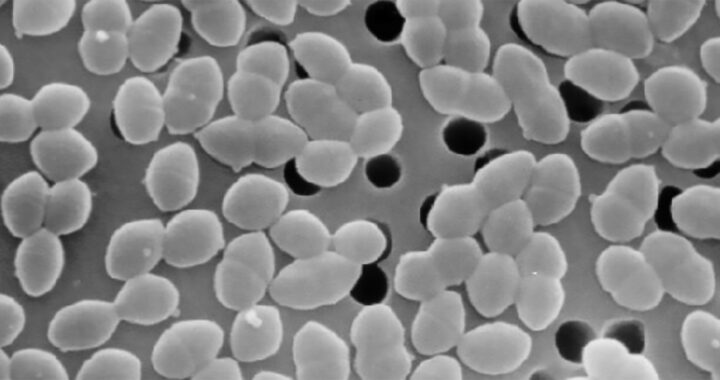
Hospitals are facing a growing challenge from drug-resistant bacteria. These bacteria have evolved new strategies to survive in medical environments. One type, vancomycin-resistant Enterococcus faecium or VREfm, has become more dominant in recent years. Scientists from the University of Pittsburgh School of Medicine have discovered that some strains of VREfm produce a bacterial toxin called bacteriocin T8 that allows them to eliminate competing strains and take over hospital settings. In their paper, which was published on 21 March 2025 in Nature Microbiology, they noted that this phenomenon is happening not only in a single hospital but also worldwide.
The Rise of Vancomycin-Resistant Enterococcus Faecium: How VREfm Strains Outcompete Each Other
Bacteriocin T8 and the Evolution of VREfm
Scientists E. G. Mills et al. analyzed 710 VREfm samples from a large hospital. Their study covered the years 2017 to 2022. The results showed that two strains, ST80 and ST117, became dominant by the end of the study period. These strains had acquired the ability to produce bacteriocin T8. This antimicrobial toxin helped them kill other VREfm strains and secure resources for reproduction. Over time, other strains disappeared, leaving only a few dominant ones.
The emerging Enterococcus faecium strains encoded a bacterial toxin called bacteriocin T8. This toxin gave them a competitive advantage over other older strains. Specific experiments confirmed that bacteriocin T8 helped these new strains outcompete others in various laboratory conditions or settings and mouse gut colonization experiments.
Furthermore, to confirm whether or not this was a local phenomenon, the team examined a global collection of more than 15631 VREfm genomes obtained between 2002 and 2022. They discovered that the same trend was occurring in hospital settings across the world. The previously dominant ST17 lineage had been replaced by ST80 and ST117 lineages or bacteriocin-producing strains. This confirmed that bacteriocin T8 was a key factor in the evolution of VREfm.
Impacts on Hospitals and Patient Safety
The resistant strains of Enterococcus faecium are one of the most difficult hospital-acquired infections to treat. It causes serious infections. Immunocompromised patients are at higher risk. The ability of certain strains to eliminate competitors means they can spread more easily. Once these strains establish themselves in a hospital, they can persist for long periods. This increases the risk of outbreaks and complicates infection control efforts.
However, although the emergence of bacteriocin-producing VREfm strains does not appear to make infections more severe, it does make the bacterial population more uniform. This could create new challenges for treatment. Specifically, even if only a few dominant strains exist, this bacterial species may become easier to target with new therapies, and at the same time, their resilience could make them harder to eliminate completely.
Several workarounds have been put forward. Scientists are now exploring ways to use bacteriocins as treatments. For example, since bacteriocin T8 is highly effective at killing other bacteria, it may be possible to harness its properties for medical use. Some researchers suggest developing bacteriocin-based antibiotics. Other researchers are proposing using bacteriophages, which are viruses that infect bacteria, to target resistant strains.
FURTHER READING AND REFERENCE
- Mills, E.G., Hewlett, K., Smith, A.B. et al. “Bacteriocin Production Facilitates Nosocomial Emergence of Vancomycin-Resistant Enterococcus Faecium.” In Nature Microbiology. DOI: 1038/s41564-025-01958-0